
Denied Medical Claims Management
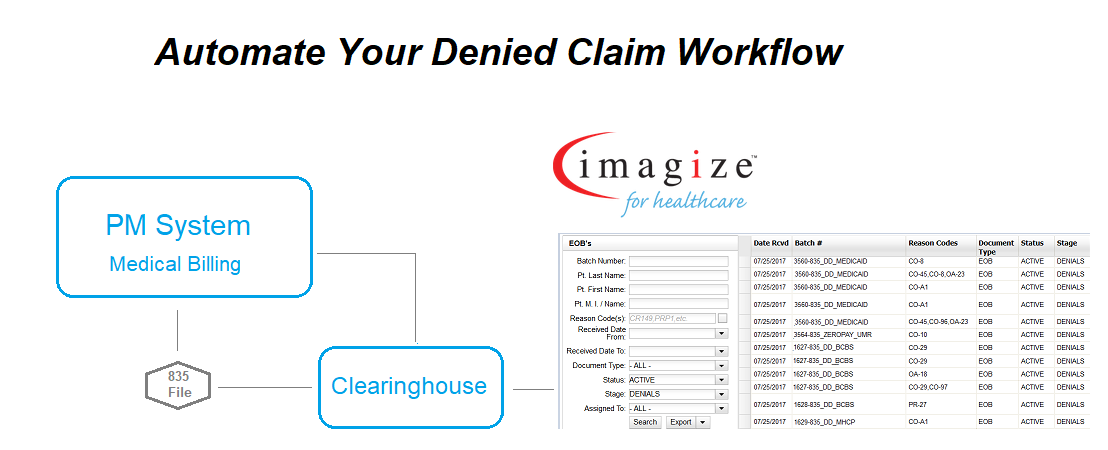
Denied medical claims are quickly identified and tracked in imagize while working alongside your EHR and practice management system. Each denied claim is immediately tagged and placed in easy-to-use work queues to review and resolve. High priority claims are filtered and listed based on urgency, critical timelines, dollar amounts, etc. ensuring each claim is properly managed and quickly resolved.
Easily Track Denied Claims
Gain efficiency and improve productivity with a powerful and easy-to-use denied medical claims management system. imagize automatically sorts and tags denied claims based on timelines, financial data and other important claim information.
- Eliminate delays and lost revenue
- Improve daily deposit totals and cash flow
- Managed and obtainable workloads
- Claim balance and open status reports
- Productivity and efficiency tracking
Eliminate Manual Reports
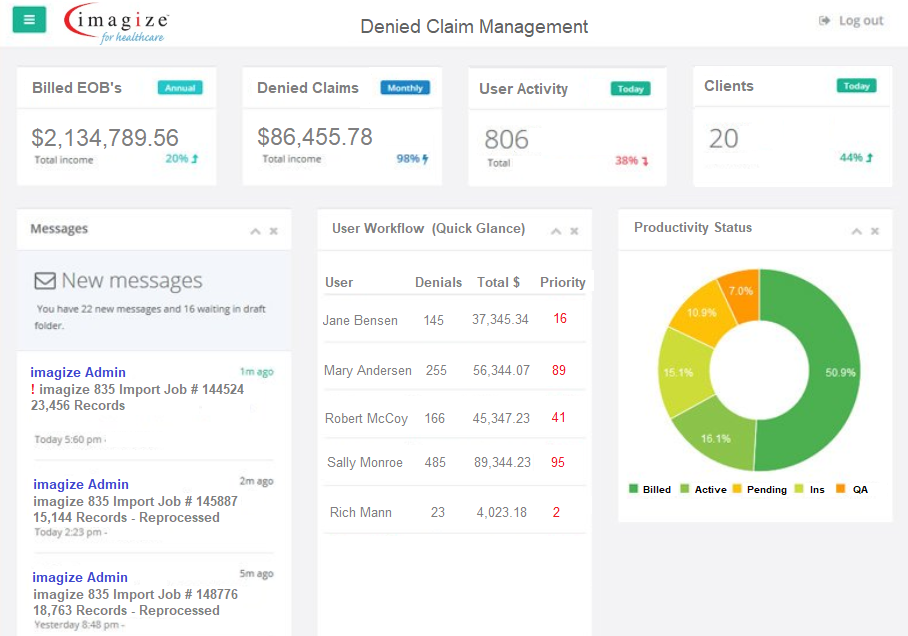
Important metadata for each claim is stored allowing imagize to prioritize, report, and provide real-time status on a variety of criteria.
- Intuitive dashboard provides real-time status
- Easily identify unpaid claims
- Quickly manage and resolve priority claims
- Monitor user activity and workload
- Multiple reports for daily activity
